Partner to Decide
⌛ ~3 min read
Project Info
Role: Lead UX Designer
Timeline: 3 months for research and design
Launched: 2023
Impact
Secured White House Blueprint funding
Adopted in 2024 by Boston Medical Center, Minnesota Community Care, and the UC San Diego Health System
The Challenge
"Shared decision-making" in healthcare sounds great on paper—two people sitting together, weighing medical options like rational adults.
The reality is far messier.
It was just routine, like I was just another patient for the day. He would ask, 'Do you have any questions?' But I felt so rushed that I would say 'No, I don't' and completely forgot the questions.
– Participant 3
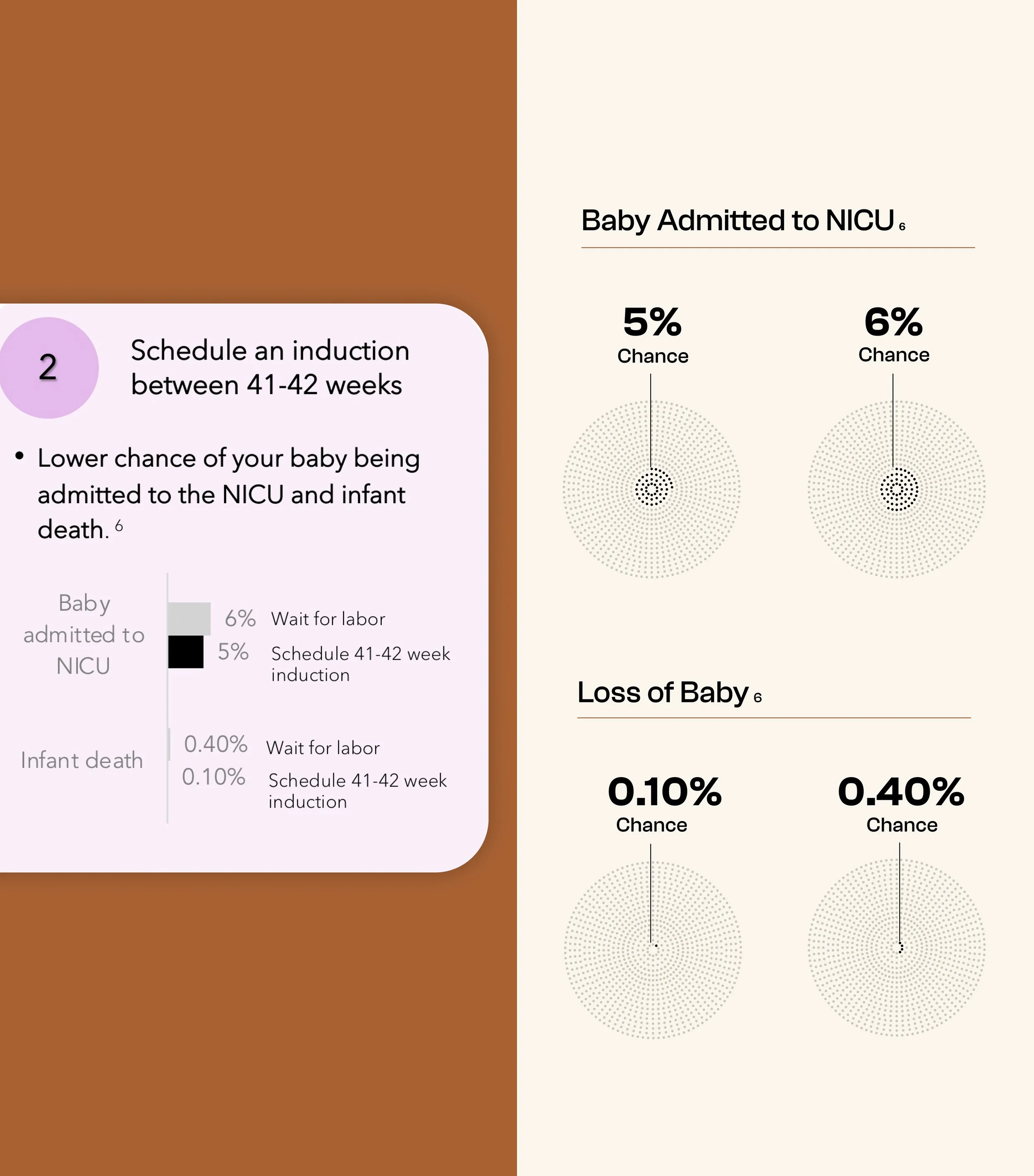
Labor induction affects 1 in 4 pregnancies, yet most people make this decision feeling rushed and unprepared.
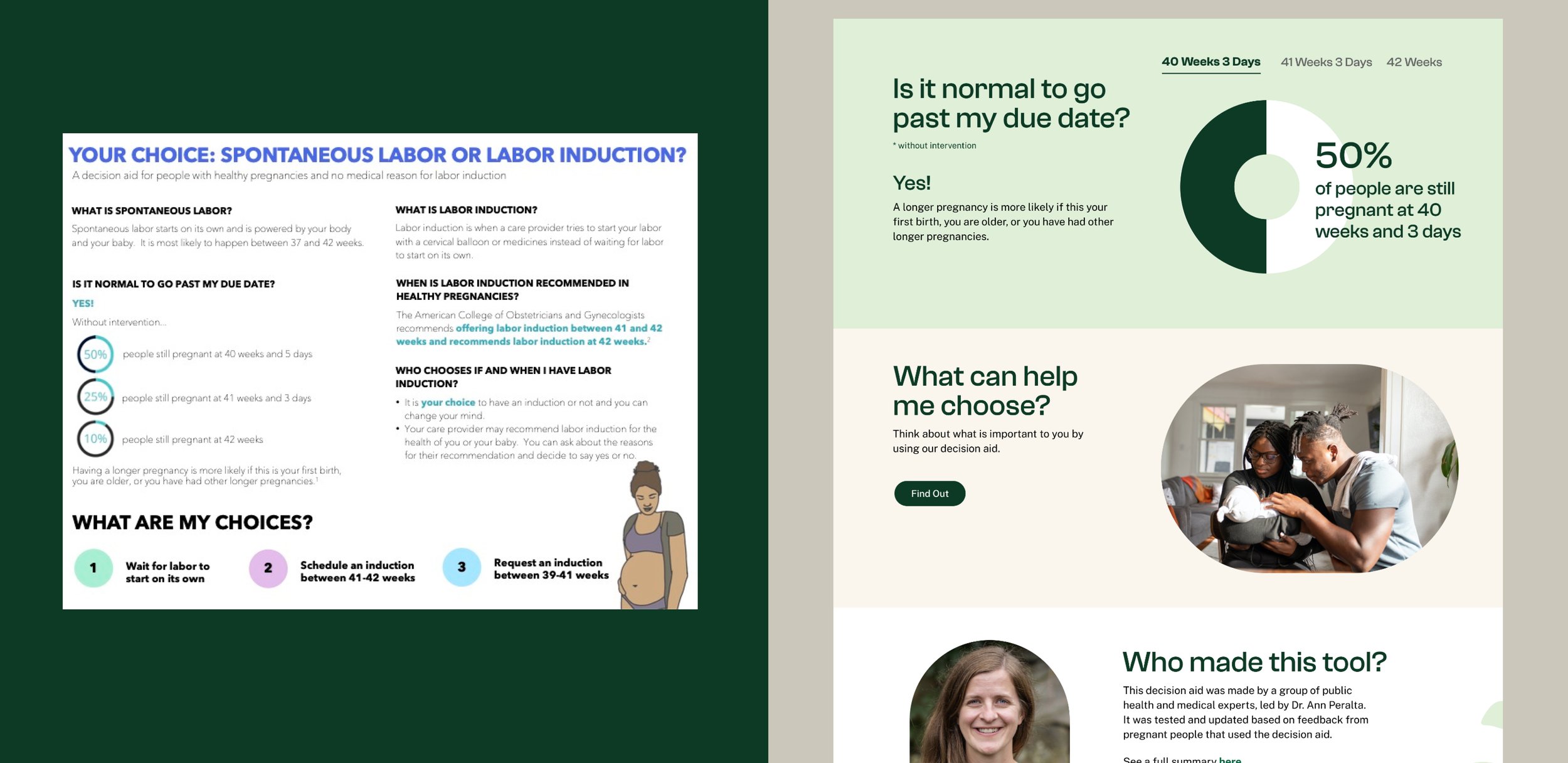
Partner to Decide, a nonprofit focused on equitable maternity care, had already created an evidence-based decision aid to solve this problem. But it was stuck in paper format, limiting their ability to reach the marginalized communities who needed it most.
The core challenges I needed to address were both technical and deeply human:
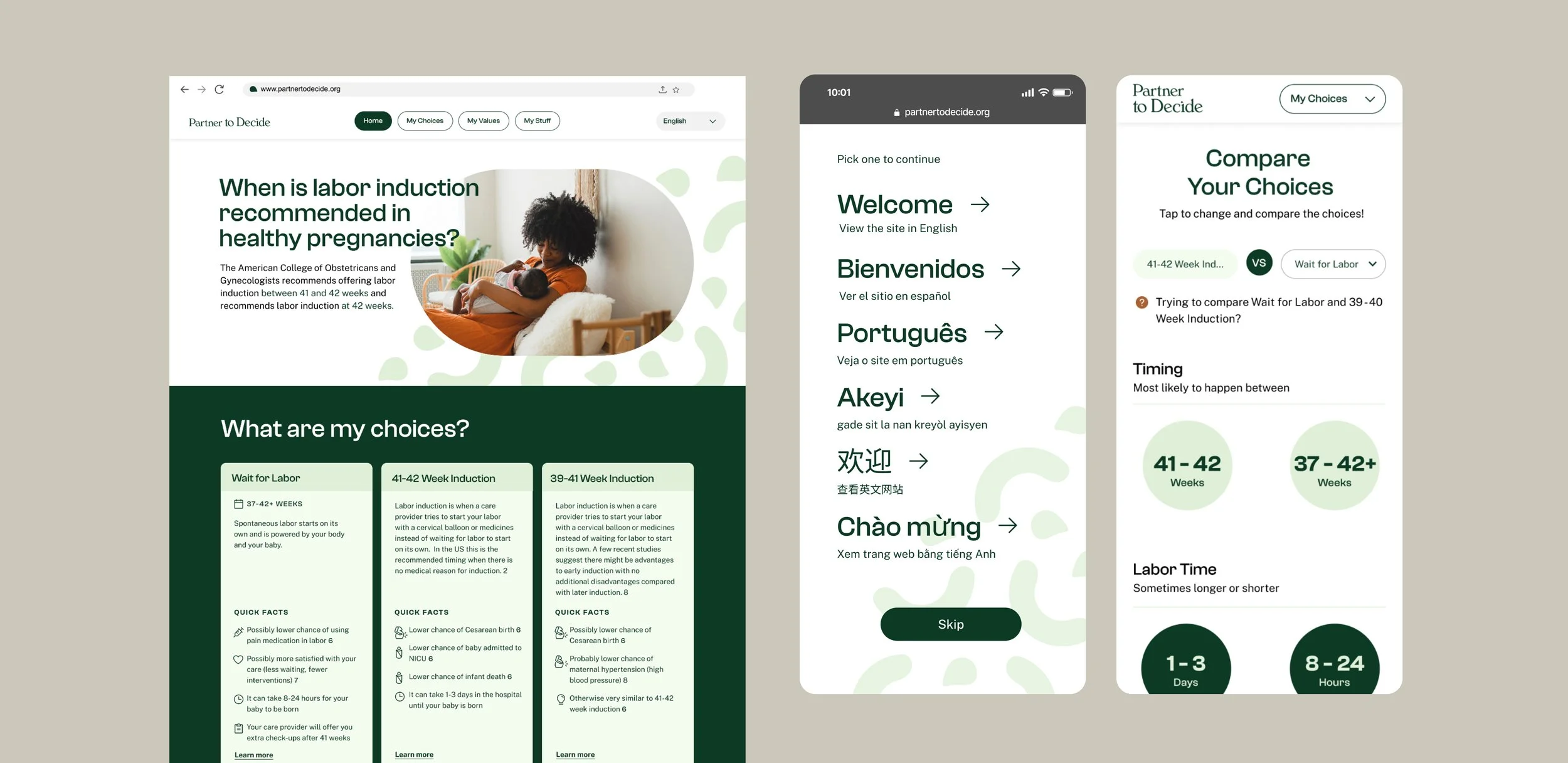
Equity: Creating accessible experiences for diverse literacy levels and language needs
Clinical credibility: Building a digital experience trusted by both providers and patients
Technical constraints: Delivering high-impact features within a tight 3-month timeline while coordinating with an external development team
Combat stigma: Providing unbiased, credible information that could transform how people traditionally explore induction options
My Process
Discovering the Real Problem
I started by shadowing 11 interviews with pregnant individuals, new mothers, and labor nurses. What we discovered changed everything we thought we knew about what people actually needed.
What we found is that people didn't need more information crammed into appointments — they needed accessible education they could absorb on their own timeline. This allowed the precious 15-minute appointment to focus on what matters: personal values and priorities that are impossible to rush through.
This insight guided my UX inspiration audit of 10+ existing decision aids and healthcare websites, where I specifically looked for information hierarchy solutions, progressive disclosure patterns, and conversation-facilitation features that could bridge the gap between self-learning and provider discussions.
Designing with Constraints
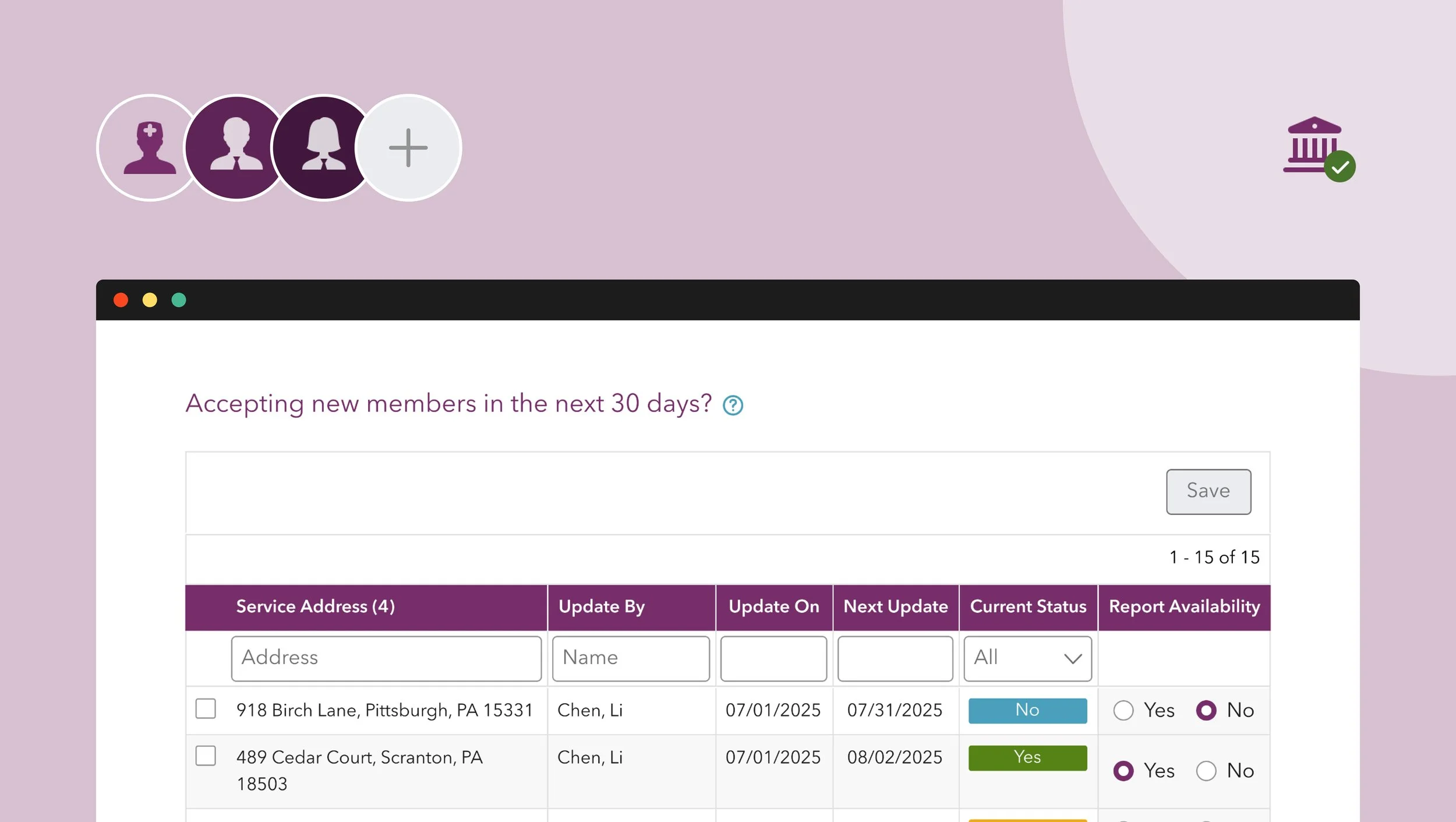
Working with a tight 3-month timeline and external developers meant every feature decision mattered. I led a co-creation workshop with other designers using "How might we" prompts to brainstorm features inspired by our research and audit findings.
From 12 initial concepts, I conducted a priority circle workshop to narrow down to 3 high-impact, feasible features for the MVP.
🟢 What made the cut:
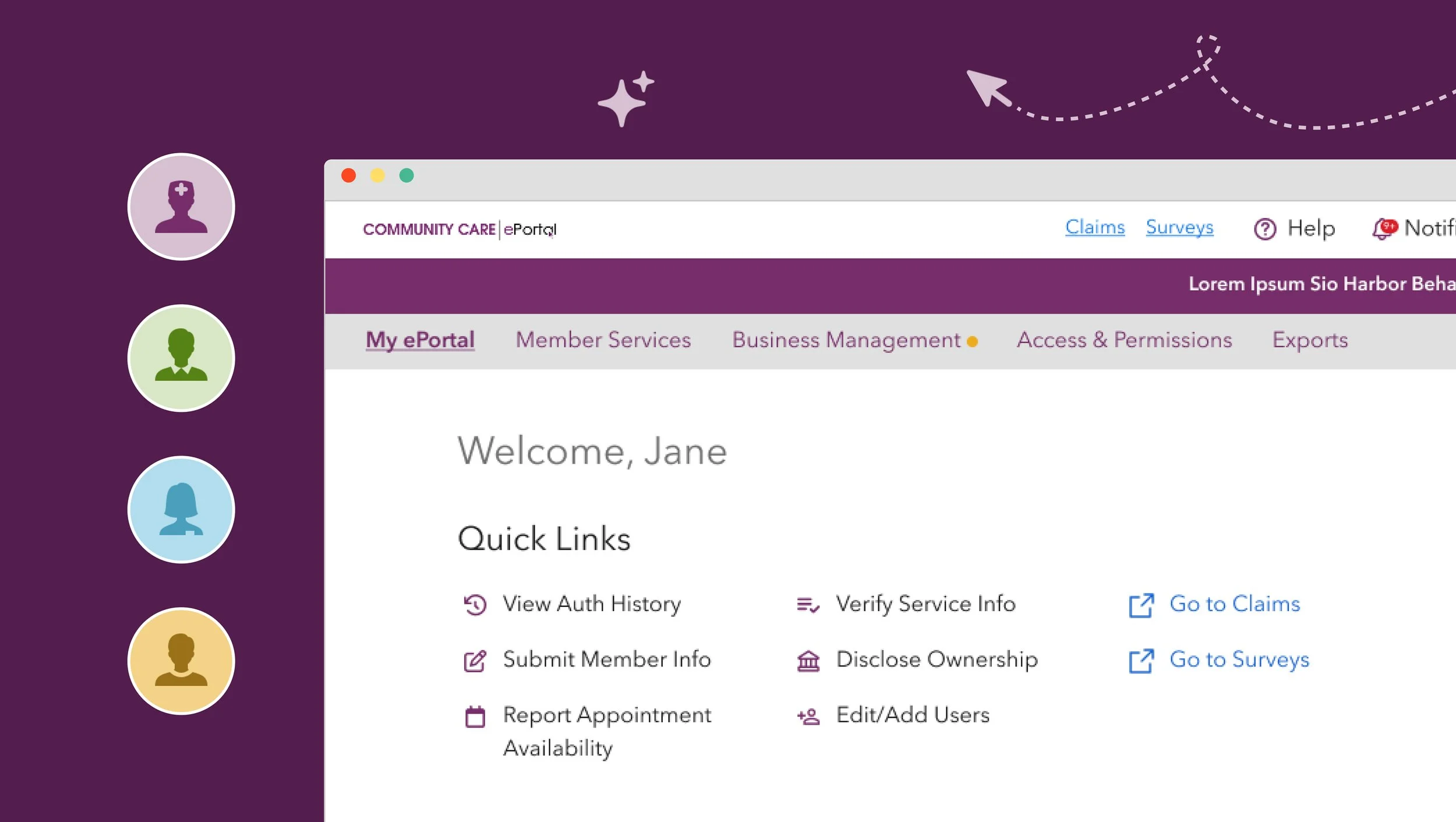
My Choices: Addresses the need to compare options at a glance while leveraging existing content
My Values: Transforms the decision aid's value clarification table into an interactive quiz
My Stuff: Captures quiz summary and questions to better prep for appointments
🔴 What didn’t: Community-based features (e.g., discussion forums and polls) and AI chatbot functionality were deemed out of scope due to development complexity, maintenance effort, and are less critical to decision-making.
Testing With Users
I created two prototype experiences and tested them with 10 diverse participants. "The Advocate" focused on personal advocacy, while "The Researcher" focused on information deep dives.
What I didn't expect: contrary to my assumption that experienced mothers would prefer the advocacy approach and first-time mothers would gravitate toward research, everyone followed the exact same learning sequence—why induction → compare options → check values. This finding led me to integrate the two prototypes into one guided flow that felt natural and met users where they were.
Success metric: All 10 participants said they felt "much more prepared" and "confident" after using the new decision aid. That kind of unanimous feedback told me we'd hit something meaningful.
A key pivot happened when I watched two participants react poorly to heavy statistics appearing without warning. That led me to add expandable cards with content warnings, giving users control over when they encountered sensitive data.
Results That Matter
Since launching in 2023, the new digital decision aid has gained strong institutional support:
White House Blueprint funding secured
Adopted in 2024 by Boston Medical Center, Minnesota Community Care, and UC San Diego Health
Silver Anthem Award 2024 for health education innovation
More importantly, pregnant people now enter provider appointments feeling informed and confident rather than rushed and anxious.
What I Learned
Design systems matter — even basic ones. Despite detailed annotations, inconsistent styling across breakpoints highlighted gaps in our external developer handoff.
Content governance is critical — establishing a single source of truth upfront would have prevented time-consuming prototype updates and ensured translation consistency.
Emotion drives healthcare UX — pregnancy is deeply personal. Designing for the emotional journey is just as important as educating future moms. This project proved that the best healthcare experiences happen when you design for human vulnerability, not just clinical efficiency.